What procedures and tests are carried out before the operation of total knee replacement?
Usually about 7-10 days prior to surgery, some blood tests and examination of urine and medical check up by a physician are carried out to make sure that you are fit to undergo the operation and are otherwise in good general medical condition. Urinary tract infections are common, especially in older women and need to be treated before surgery. Teeth need to be in good condition. An infected tooth or gum, infection in urine or infection anywhere else in the body like infected toe nail or a skin lesion may also be possible sources of infection for the new knee.
When do I have to get admitted to the hospital and what happens after that?
You would be admitted to the hospital on the evening before the day of operation and would be examined again to make sure that you are fit and well to undergo operation. The anaesthetist would see you for preoperative assessment and would explain to you the anaesthesia procedure.
What kind of anaesthesia would be used for the operation? Will I get a lot of pain after the operation?
Two types of anesthesia are commonly used for knee replacement surgery. The first type of anesthesia (Spinal and epidural anesthesia), which is very commonly used, works by numbing your legs so you do not feel the operation. This is done by placing numbing medicine around the nerves that go to your legs using a small catheter in your lower back. You are also given medicine to relax you and you may fall asleep, but you can still breathe on your own. The potential advantages of this anesthesia include less blood loss and less risk of lung problems and blood clots in the legs. Also, the epidural can be continued after your surgery to help control the pain. The second type of anaesthesia is a general anesthesia, which puts you in a deep sleep and therefore requires assistance with your breathing. The risks are small and usually are related to the heart or lungs.
Would I require a blood transfusion during or after the operation?
This will depend on your level of haemoglobin before surgery. If it is normal, you may not require blood transfusion after surgery.
How long does the surgery last?
The actual surgical procedure usually takes approx. 1-1½ hours. However, preoperative preparation, time required for the anesthesiologist to prepare you for surgery and then following surgery to transport you from surgery to the recovery room may make your operating room and recovery room stay longer.
Will I get a lot of pain after the surgery and while doing physiotherapy?
It is very likely that you will have pain in your knee. This is normal and you should not be surprised or concerned. Most of the pain that you experience right after surgery is from the surgical incision and dissection. You will be given strong pain medication through your I.V. line and also through the epidural catheter and most of the patients are very comfortable with these pain relieving measures. The pain will decrease over the first couple of days.
You will not get much pain while doing exercises and most of the patients stop taking pain relieving medicines by the end of 3rd or 4th week after surgery. It is helpful to take pain killer an hour before physiotherapy to help you do exercises better without much pain and gain the knee motion quickly.
What happens after surgery?
After surgery you will be taken to the Recovery Room for a period of close observation, usually for 2-3 hours. Your blood, pressure, pulse, respiration and temperature will be checked frequently. Although circumstances vary from patient to patient, you are likely to have some or all of the following after surgery:
1) You will find that a large dressing has been applied to the surgical area to maintain cleanliness. This dressing is usually changed on the next day after surgery by the surgeon.
2) A hemovac suction container with tubes leading directly into the surgical area enables the nursing staff to measure and record the amount of drainage being lost from the wound following surgery. The hemovac is usually removed by your doctor on the next day after surgery.
3) An IV, started prior to surgery, will continue until you are taking adequate amounts of fluid by mouth. Antibiotics are frequently administered every eight hours, until all drains are removed, to reduce the risk of infection.
4) One side effect of anesthesia is often a difficulty in urinating after surgery. For this reason, a sterile tube called a catheter will be inserted into your bladder to ensure a passageway for urine. This may remain in place for 2-3 days.
5) Diet: You will be allowed to progress your diet as your condition permits; starting with ice chips and clear liquids to diet as tolerated.
6) You will be assisted into the chair the second day after surgery provided there are no complications. Physical therapy is started the morning after surgery. It is very important for you to have pain medication 30 minutes before going to physical therapy to help you fully participate in exercises.
7) How well you regain strength and motion is, in part, dependent upon how well you follow your physical therapy. This part of your rehabilitation is something that you must do for yourself, and not something someone else does for you. If there are no complications after surgery, most patients stay in the hospital for approximately 3-4 days.
8) You are ready for discharge from the hospital when you are able to drink and eat without upsetting your stomach and you don't require any medications that need to be administered through an I.V. line. You need to be able to sit in a chair, stand up, and walk about 30 feet. In order to be discharged there cannot be any evidence of infection, blood clots, or other complications.
What happens after I go home?
1) You will be sent home on prescribed medications to control pain. Plan to take your pain medication 30 minutes before exercises.
2) Continue to walk with walker/stick. Bear weight and walk on the leg as much as is comfortable. Walking is one of the better kinds of physical therapy and for muscle strengthening.
3) If excess muscle aching occurs, you should reduce your exercises.
4) Put ice packs on your operated knee, 3-4 times daily to reduce pain and swelling. When using ice, remember not to get your incision wet before your staples are removed.
5) Keep the incision clean and dry. If you observe sudden increase in swelling and pain, drainage from the incision site, redness around the incision, or fever is noticed, report this immediately to the doctor.
6) You should not take bath until after staples are removed. Generally, the staples are removed in two weeks.
7) You should not drive a car until after the 6-week follow-up appointment.
For how long, would I be required to do physiotherapy?
Continue the exercises shown to you until about 2-3 weeks after surgery, when you may be required to go to a physical therapy facility on an outpatient basis.
Remember, there are really only 4 goals for rehabilitation following total knee replacement.
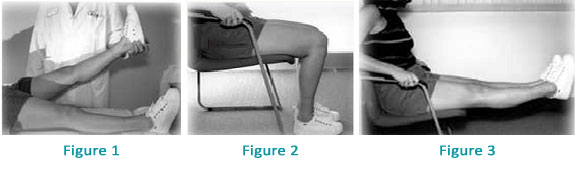
1) The knee must come out completely straight in full extension as shown in Figure 1.
2) The knee must bend to at least 90° and preferably to 120° as shown in Figure 2.
3) The quadriceps muscle must regain strength to actively extend the knee as shown in Figure 3.
4) You should be able to walk as far as you want without a cane or crutch.
What can I expect from an artificial knee?
An artificial knee is not a normal knee which the nature has provided. However, the operation will provide pain relief for at least 12-15 years. In many patients, their total knee replacement will last their lifetime, but in some, it may not last that long. If replacement provides you with pain relief and if you do not have other health problems, you should be able to carry out most of the normal activities of daily living like unlimited standing, sitting, walking etc. You can do exercises like bicycling, walking and swimming. However, activities that overload the artificial knee like jogging and sports like tennis must be avoided to increase the longevity of the artificial knee. Most of the patients with stiff knees before surgery will have better motion after a total knee replacement.
There are so many different types of knee joints available in the market. Which one is the best suited for me?
Almost all modern total knee implants have very similar basic Total Condylar design and have some minor differences in their design. Some of the joints have metallic components fixed to the end of thigh bone(Femur) and Leg bone (Tibia) with bone cement and a plastic insert between the two metallic components (Metal backed Tibial component). It offers some technical advantage to the surgeon. As against this, some other designs have All-Polyethylene tibial component called all-poly tibia where the femoral component is metallic and the tibial component consists of only plastic. All-poly tibial base plates are more cost effective to the patient. Some of the other available knee implants include gender specific knees particularly for female patients and high flexion knee designs (Hi-flex knees) which are supposed to provide more knee bending. Long term results regarding longevity and patient satisfaction for these relatively recent designs are, however, not available at this stage. Therefore, the final choice of the implant should be ideally left to the operating surgeon who would base his decision keeping in mind the requirements of the patient, suitability of a particular implant in the given patient, survivorship (Longevity and track record) of the implant and also his experience and familiarity with the instrumentation and implant.
How long do artificial knees last? Then What?
In many ways, a total knee replacement is similar to a set of automobile tires. How long the knee replacement lasts is related to the type and amount of use, and not simply how long it has been implanted. A set of automobile tires can last for many years if the car is not driven very much or they can wear out in less than one year if they are driven many miles over rough roads. How long a total knee lasts depends on how much it is used, what types of activities it is used for, how heavy the patient is and whether the patient is staying in good physical condition. In many patients, their total knee replacement will last their lifetime and in others, it may not. Total knee replacements are designed to provide painless and unlimited standing, sitting, walking, and other activities of normal daily living. They do very well for walking, bicycling and swimming. They are not designed for jogging or sports like tennis and skiing. Total knee replacement surgery is done to improve quality of life and each patient must decide for himself what makes life worth living for them and pursue happiness through those activities. You should be aware, however, that the longevity of a total knee replacement may be shortened by frequent, vigorous activities.
In the event that a total knee fails, it is possible to implant another knee. Such revision total knee replacement surgery may be a lesser or greater operation than the original total knee surgery. In general, the results of revision total knee surgery are not quite as good or predictable as for primary total knee replacements. Following revision total knee replacement, most patients have good relief of pain and are able to walk as far as they desire.
Is there any role of computer assisted surgery (CAOS) ?
Total hip and knee replacement are very reproducible and successful surgeries .Computer-assisted surgery aims at increasing the precision of implant positioning. Though it is supposed to improve the precision of the surgery, it is not known whether using these systems will result in a better long term survival of the prosthesis. Because this technology is new, expensive, and adds time to the surgical procedure, it has not been widely adopted. As CAOS is used and studied, its utility and value will be better understood. Longer and more comprehensive follow-up studies are needed to better understand the indications, limitations and complications of this surgical technology.
For further information, http://www.aahks.org/patients/resources/CAOSpositionstatement.pdf
Should I opt for high flexion knee joint replacement to allow me to sit cross legged and squat?
With most of the current designs of the conventional total knee replacements, 100-125 degrees of knee bending (flexion) is achieved which is sufficient to perform most daily activities like walking, climbing stairs, getting in and out of car or rickshaw, rising from a chair etc. However, if your routine daily activities involve kneeling, squatting and sitting cross legged , a high flexion knee joint can be implanted. However, it is not known whether efforts to increase flexion could cause deleterious effect on the implanted joint like early loosening. One should, therefore, be careful about indulging in activities which cause extreme flexion of the knee joint. Also, there are certain criteria which have to be fulfilled for the implantation of the high flexion designs to achieve more than average range of motion of the knee joint after surgery.
Is there any harm by waiting too long for surgery?
As the knee arthritis worsens, the stiffness of the arthritic joint also worsens. This can make the replacement surgery technically more demanding. It may also lead to a longer recovery period and more physical therapy. In severe cases, joint flexibility may never return to normal. By waiting too long, you may not get the full benefits of your knee replacement surgery and such a delay could negatively impact the result of the surgery.
Am I too old to undergo a knee replacement surgery?
Knee replacement surgery can be carried out even in patients who are above the age of 75-80 years provided they are medically fit and are in good general health and their activities of daily living is restricted by painful arthritis of knee joints.